Source: NWO.nl February 15, 2023 Text: Sonja Knols
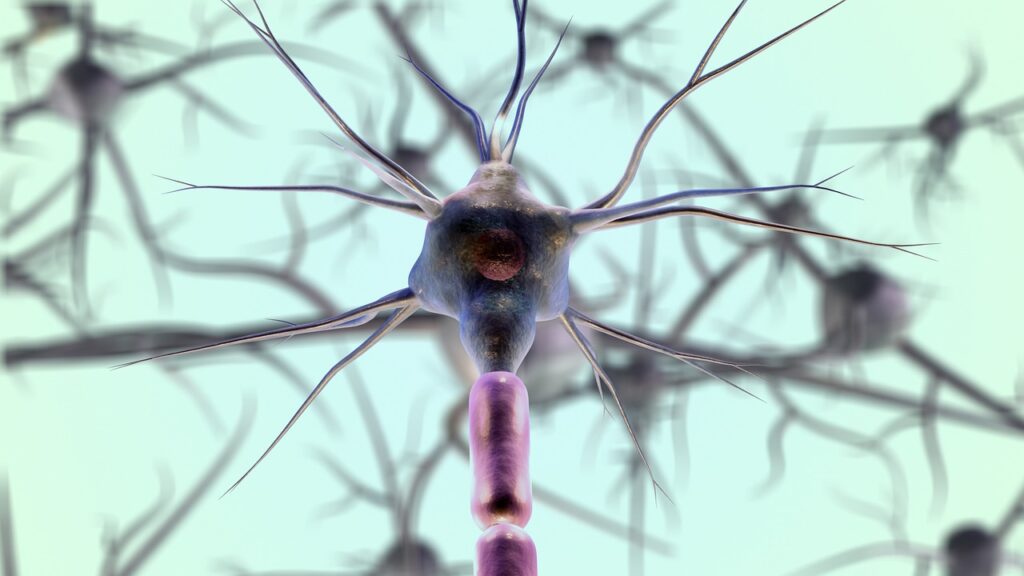
How do electrical signals travel through our nervous system? And how can we intervene to do something about conditions such as chronic pain, hearing impairment or spasticity? In the NeuroCIMT Perspective program, engineers, clinicians and companies investigated the control function of the central nervous system to offer patients a better quality of life.
The researchers focused on four different neurological and sensory disorders, namely hearing problems, pain regulation, blood pressure regulation and movement control. They did this in eight separate, interconnected projects. “The common thread within NeuroCIMT was the organization of the human nervous system,” says program leader Frans van der Helm, professor of Biomechatronics and Bio-robotics at TU Delft. 'To prevent tunnel vision, we studied different systems and looked for similarities and differences. The idea was that if you understand how signals from the auditory nerve are processed by the brain, you might also better understand what goes wrong in patients with chronic pain.' Using various techniques, the researchers have mapped out how the brain processes signals from different nerves come.
Fruitful cross-pollination
Despite the individual focus of the eight different projects, there were clear cross-pollinations, says Van der Helm. 'For example, a number of researchers were connected to multiple projects, and we used techniques from one project in the other.' One of those techniques was developed within the NociCept project, aimed at the pain regulation system.
Sometimes patients are told that their pain is 'in their head'. We see in measurements that this is literally the case
Tom Berfelo, technical medical researcher St. Antoniusziekenhuis
Tom Berfelo, a technical medical researcher at the St. Antonius Hospital in Nieuwegein, explains: 'Within NociCept we develop a diagnostic to objectively map the function of the pain system. You cannot measure pain properly. We are still dependent on subjective information: the patient himself rates the pain at that moment. We want to have physical and neurophysiological biomarkers that objectively describe the pain. We have developed a method for this that allows us to see how pain signals are processed. By applying small electrical stimuli directly to the pain fibers in the skin, we activate the pain system. We then look at how this signal arrives in the brain by, among other things, EEGs (studies that reflect the electrical activity of the brain, edstudies that reflect the electrical activity of the brain, ed
Chronic pain measurable
Although the research is still in the exploratory phase, in which the scientists first want to see whether this measuring method is at all suitable for patients in a hospital environment, the first results are positive, says Berfelo. 'In comparative studies we see clear differences between patients with chronic pain and healthy subjects. Sometimes patients are told that their pain is “all in their head”. We see in measurements that this is literally the case: something measurable happens in their brains that differs from what happens in healthy control subjects. The next task is to explain the cause of these differences, for example by relating what we see to underlying pain characteristics. We want to get an idea of what causes these changes in the pain system and investigate how we can treat them.'
Understanding speech in noisy environments
This method of creating electrical pulses with very specific fingerprints, which can then be found in the EEG of the brain, is much more widely applicable, says Van der Helm. The same technology was also used in the Otocontrol project, in which the researchers were looking for new solutions for hearing impaired people who use a so-called cochlear implant. This is a device that converts sounds into electrical pulses, which stimulate the intact part of damaged auditory nerves via implanted electrodes.
“Although these implants can achieve 100 percent speech recognition in otherwise quiet environments, understanding speech in noisy environments remains a challenge,” explains Josef Chalupper, principal research engineer at project partner Advanced Bionics, from. “The main goal of the project was to create an objective, automated system that generates appropriate stimulation patterns, measures the resulting signals in the patient's brain, and then finds the optimal settings for that person's hearing aids.”
Hearing test
And although that end goal has not yet been achieved, important steps have been taken in the right direction, Chalupper believes. 'We have developed several new methods that help characterize individual patients. In the short term, we now have a hearing test that people can do at home on their mobile phone to prepare for or even replace a visit to the clinic. For the medium term, we have a method that allows us to distinguish between the signals placed on each of the sixteen electrodes of the implant. This allows us to optimize the stimuli that we apply to the auditory nerves. And for the long term, we have taken the first steps toward reading the brain and finding auditory fingerprints that are crucial for listening tasks.”
New measuring techniques essential
At the moment, the human brain is still largely terra incognita, Van der Helm teaches. 'We may only know 1 percent of them. There are many places in the brain where you cannot measure. The development of new measuring techniques is therefore essential.'
External measurements such as an EEG are complicated, he emphasizes. 'The signal you measure is the result of all kinds of different processes. The trick is to unravel which part of that signal is caused by the process you want to study. Within NeuroCIMT we have taken a number of new steps that now allow us to better calculate what caused a certain signal. I like to compare it with seismograms, from which you can determine the location of the source of an earthquake.'
Knowing what doesn't work
Although most of the eight projects have produced important progress towards prototypes of new medical technology, there is also a negative result that the project leader wants to highlight as an important outcome. 'The iDTCS project investigated the hypothesis that sending a direct current in a very targeted manner through certain brain areas could improve the ability to learn new techniques. However, we have not found any evidence for this, so it simply does not work.'
Important progress
All in all, Van der Helm is very satisfied with the results of the program. 'We have made important progress in several areas. In addition to new insights into how the brain processes signals, an orthosis has also been developed for people with a spastic calf muscle. By using a spring with negative stiffness, the patient gains more control over the spastic behavior. This idea should work for other muscles too. A follow-up project has been started on this.'
Need for large-scale patient studies
All partners involved in the NeuroCIMT program are part of a very active public-private consortium, the Innovative Medical Devices Initiative Centers of Research Excellence Caretech, in which the former IMDI Centers Neurocontrol and SPRINT have been merged. In addition, several partners are part of Neurotech-NL, a partnership that develops new methods of neurostimulation.
Van der Helm still has one concern. Getting such technology into the clinic requires large-scale patient studies, for which research funding is difficult to find. 'And the companies in this sector are often SMEs. They don't have the time or resources for this. This situation is holding back many developments, and that is a shame in these times of an aging population and increasing healthcare costs.'
